Why it Matters
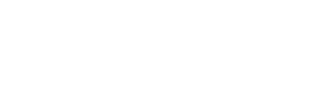
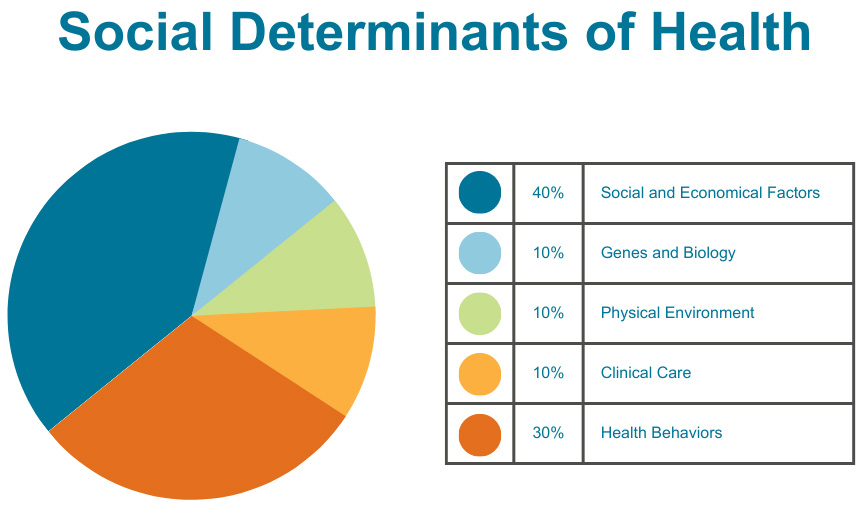
The Social Determinants of Health (SDH) are the conditions in which people are born, live, work and age. They are shaped by the distribution of money, power and resources at global, national and local levels. SDH account for an estimated 60 percent or more of health outcomes and are largely responsible for health inequities. Social factors influence both an individual’s physical environment and health behaviors. To achieve health equity, where everyone has a fair and just opportunity to be as healthy as possible, it is essential to address the social determinants of health.
Community health centers provide numerous services which address the social determinants of health including transportation, housing support, peer support groups, and food programs. Screening for social needs is a powerful mechanism to identify individual patient needs and provide support and services to address these concerns. Additionally, screening helps community health centers develop targeted interventions, improve care coordination and patient engagement, and make better use of partner/enabling services.
Social needs are shaped by the broader social factors – or determinants – in people’s lives. Beyond screening for needs, CHCs also serve as advocates to shape policy and structures that perpetuate health inequities. By moving upstream, CHCs serve as a catalyst to disrupt this cycle and prevent disease and poor health outcomes.
OPCA’s Health Equity & Social Care Work
National
Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE)
OPCA partners with the National Association of Community Health Centers (NACHC) and Association for Asian and Pacific Community Health Organization (AAPCHO), to develop and roll out a standardized social needs screening tool for community health centers nationwide. PRAPARE is both a protocol and a tool to help care teams collect the data needed to better understand and respond to patient’s social needs, and is the dominant social needs tool used in health centers today.
Membership
In partnership with the Oregon Health Authority, OPCA’s APCM program increases flexibility for community health centers to focus on developing a more effective approach to improving population health. APCM allows health centers to understand and respond to the non-medical circumstances that influence their patients’ needs and priorities, which may be best addressed outside the examination room and even outside the walls of the clinic.
OPCA developed a curriculum called Empathic Inquiry, a conversational approach to social needs screening to promote partnership, affirmation and patient engagement through social needs screening.
Statewide
OPCA collaborates with Oregon health centers, partners, and policy makers to shape public policy to achieve health equity for all Oregonians.