
WELCOME TO OPCA’S 40TH ANNIVERSARY ANNUAL REPORT
ROOTED IN COMMUNITY, CULTIVATING HEALTH EQUITY
Our Core Identity: A Gathering Place for Community Health Centers
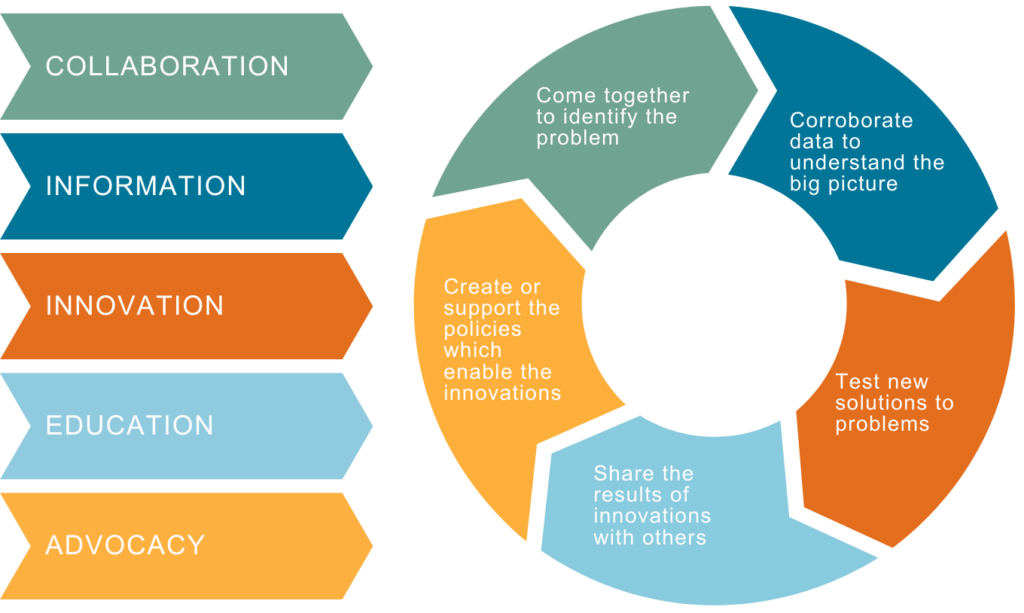
For federally qualified health centers in Oregon, OPCA is a gathering place for learning new skills, building community, and sharing ideas. Together, we collaborate to create health equity in communities across the state. As an organization, OPCA follows in the footsteps of national community health movements and we support the efforts of our members as they strive to create innovative, effective, and cost-efficient health care systems that address the individualized needs of patients while maintaining state, regional, and national standards of care.
In the last 40 years, OPCA has continually grown and evolved to fit the needs of our members. In the beginning, we focused on training and technical assistance to make sure our members had access to best practices. As we grew, we added advocacy to our work to address systematic shortcomings. Public health funding has remained tight over the years, so we added payment innovations to make the best use of limited resources. Throughout our history, data has been an essential part of how we support payment innovation and advocacy, and it’s essential to the next phase of our growth as an organization. To that end, we recently adopted cutting-edge practices and the Arcadia data platform to make the most of the information we collect. Outside of our traditional areas of expertise, in 2023, we integrated with Oregon AIDs Education and Training Center (AETC) to address specific issues in population health.
As we work to cultivate health equity, sometimes we focus on the trees. Other times, we focus on the forest. Ultimately, we seek to share the stories, information, and transformational innovations which will help us solve the problems our members face each day in their pursuit of health equity.
Please enjoy the stories and information contained here in our Annual Report, and please get in touch with any questions or suggestions.

Table of Contents
- Our Core Identity: A Gathering Place for Community Health Centers
- Remembering Our Roots
- Key Health Equity Moments in Oregon and Beyond
- How We’re Branching Out: OPCA’s 3 Year Strategic Plan
- OPCA Revenue and Support
- New Cost-Savings Initiatives
- Where Innovation Sprouts: OPCA Peer Groups
- Inspired by Peer Group, OPCA Authors SB 608
- AETC & OPCA Cross-Pollinate
- APCM and Oregon’s CHCs: A 10+ year retrospective
- The Oregon Network For Community Health Centers Earns Approval for MSSP
- Sustaining Our Communities
- Stay informed.
Remembering Our Roots
A Welcome Message from Executive Director Joan Watson-Patko
Our Foundation of Collaboration

As we look at the future of OPCA with optimism for what is to come, we also reflect on the work and legacy of the past forty years. It was forty years ago, when in 1984, six community health centers (CHCs) identified a need to unite their voices so they could better serve their patients. Since our founding, OPCA has been rooted in its mission and vision of achieving health equity for all Oregonians. Over the decades, we’ve grown, adapted, and evolved to address the complex challenges health centers face in delivering low cost and high-quality care to underserved communities and populations throughout Oregon.
Our services for Oregon’s health center
s began with training and technical assistance (T/TA), and while this remains central to OPCA’s work, it was recognized early on that our members also needed support in other key areas. Health centers were facing, and continue to experience, challenges that can’t be solved through training alone. OPCA built relationships with state and federal agencies so our members’ voices would be included in conversations and decisions that directly impact health centers and the patients they serve.
OPCA helped our state gather community input in drafting the Oregon Health Plan (OHP), and we fought for our members’ inclusion in Medicaid reimbursement processes. When Oregon shifted the reimbursement process to managed care organizations, OPCA sprang into action with partners at the Oregon Health and Sciences University (OHSU) and Multnomah County to form CareOregon. Together, we designed a new health care infrastructure to ensure CHC patients had administrative support on their journeys to health.
Addressing Population Health Through Payment Innovation
 Our next undertaking was to look for ways to improve population health. We learned from community health centers in Alaska that we could radically improve the entire health services delivery system for better outcomes at lower costs if we envisioned new payment and care models. Instead of charging fees for each patient visit, we could negotiate an upfront set payment per patient.
Our next undertaking was to look for ways to improve population health. We learned from community health centers in Alaska that we could radically improve the entire health services delivery system for better outcomes at lower costs if we envisioned new payment and care models. Instead of charging fees for each patient visit, we could negotiate an upfront set payment per patient.
Through years of hard work and the vision of leaders from OPCA, Oregon’s CHCs, and the Oregon Health Authority (OHA), the Alternative Payment and Advanced Care Model (APCM) was launched in 2013. APCM aligns payment and transforms care to promote optimal health and health equity. The APCM program provides community health centers with the flexibility to not just deliver health care, but to foster health in the communities they serve.
Oregon was the first state to have a Medicaid Alternative Payment Methodology (APM) for Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs). The APCM has removed the incentive to produce face-to-face visits with a billable provider. APCM’s per-member, per-month (PMPM) Medicaid reimbursement payment is a transformational shift from the traditional fee-for-service medical model. Oregon’s APCM program has become the model for other states throughout the country.
Expanding Our Canopy with New Programs
 Through relationships built and a track record of supporting health centers in T/TA, payment and care transformation, policy, and governmental affairs, OPCA continued to explore new ways to provide value to Oregon’s health centers. OPCA worked with several health center leaders and the OPCA Board of Directors to explore opportunities to support health centers in value-based pay arrangements, and through this developed Oregon’s FQHC led clinically integrated network (CIN).
Through relationships built and a track record of supporting health centers in T/TA, payment and care transformation, policy, and governmental affairs, OPCA continued to explore new ways to provide value to Oregon’s health centers. OPCA worked with several health center leaders and the OPCA Board of Directors to explore opportunities to support health centers in value-based pay arrangements, and through this developed Oregon’s FQHC led clinically integrated network (CIN).
The Oregon Network of Community Health Centers (Network) was launched in September 2020 to allow Oregon’s health centers to work together for success in Medicaid value-based care and pay arrangements. In 2023, the Network secured funding for the adoption of a data platform (Arcadia), allowing health centers and the Network to manage value-based care data. We know our ability to advocate for value-based payment models that support our ability to drive population health is dependent on our ability to organize data into information to drive value.
Throughout 2023, the Network continued to expand service offerings through the development of an Accountable Care Organization (ACO) and earned federal approval to participate in the Medicare Shared Savings Program (MSSP) Advanced Investment Payment (AIP) model beginning in January 2024.

In 2023, OPCA continued to grow and expand service offerings to CHCs by bringing the Oregon AIDS Education and Training Center (OR AETC) under its umbrella. The OR AETC provides capacity building to organizations and offers provider education to improve patient health outcomes for people at risk or living with HIV while preventing new infections throughout Oregon and SW Washington.
Back in 1984, our founding CHCs set out to share best practices and help one another navigate a complex system of government funding and regulations. Today, OPCA retains that spirit of shared learning through 11 peer affinity groups, forums for best practice and shared learning, training and technical assistance (T/TA), programs such as the APCM and OR AETC, the Network and ACO, a legislative liaison program, federal and state advocacy, governmental affairs, and a vast library of tools and resources, all to advance our mission of leading the transformation of primary care to achieve health equity for all Oregonians.
Rooted in Community, Cultivating Health Equity
Throughout our 40 years of growth, OPCA has remained committed to community-based health system transformations which lead to better care, lower costs, and the attainment of health equity. While we cannot fully predict what challenges are on the horizon, with each year we build on that foundation to ensure our members can continue to provide comprehensive high quality primary care services to any person in need.
To our members, partners, and health center supporters, thank you for the privilege of allowing OPCA to continue to work with you to achieve health equity.
In solidarity and gratitude,
Joan Watson-Patko
OPCA Executive Director
Key Health Equity Moments in Oregon and Beyond

2023 |
OPCA began housing the Oregon AIDs Education and Training Program (AETC). |
2020 |
OPCA developed the Oregon Network of Community Health Centers. |
2018 |
OPCA developed the empathic inquiry protocol as a best practice guide to build trust between patients and providers. |
2010 |
OPCA, OHSU, and OHA developed the nation’s first Alternative Payment Methodology and Advanced Care Model (APCM). |
1994 |
OPCA helped coordinate community input on the Oregon Health Plan (OHP). OPCA negotiated with the Oregon Health Authority (OHA) to ensure health centers would be reimbursed for their services. OPCA, Multnomah County and OHSU form CareOregon. |
1992 |
Congress enacted the 340B Drug pricing program. |
1991 |
The Omnibus Budget Reconciliation Act formally defined Federally Qualified Health Centers (FQHCs) for the first time and set for the standards of care. |
1984 |
Oregon community health centers banded together to form the Oregon Primary Care Association (OPCA) to coordinate their resources, ideas, and advocacy. |
1965 |
President Lyndon B. Johnson established Medicare and Medicaid programs. |
1904 |
Local women form the Portland Free Dispensary. They soon partnered with the University of Oregon Medical School (which became Oregon Health and Sciences University or OHSU). |
1854 |
Oregon’s Territorial Legislature passed the “Act Relating to the Support of the Poor,” which required counties to provide public services like food, shelter, and medical care to residents in need.
|
How We’re Branching Out: OPCA’s 3 Year Strategic Plan

OPCA Revenue and Support
New Cost-Savings Initiatives
Sponsorship Program for Annual Conference
The OPCA Annual Conference provides a unique forum for collaboration and knowledge-sharing to enhance community health throughout the state. The conference regularly draws around 150 community health center leaders and medical professionals.
In 2024, for the first time, OPCA created a process to include sponsorship opportunities at the conference. Sponsors’ contributions help OPCA provide an exceptional conference experience to our members while keeping costs low. In turn, the sponsors’ generosity and support is recognized by influential decision-makers as well as local and national health center partners.
Thank You to Our Generous Sponsors!
Together, We Raised More Than $30,000 to Support the 2024 OPCA Annual Conference
Group Purchasing Discounts for Oregon FQHCs
“Once we discovered how to unlock our program’s potential, it has not only saved us thousands of dollars but also streamlined our vendor search process!”
– One Community Health

Through OPCA’s partnership with the Washington Association for Community Health Group Purchasing Program, our members can access an array of resources including discounted pricing, new and familiar vendors, informational webinars, newsletters packed full of supply chain info, and a monthly purchasing workgroup meeting.
Group Purchasing Coordinator Terri Blazell-Wayson (twayson@wacommunityhealth.org) can assist your center by answering questions, helping you find services or supplies and connecting you with other purchasing staff.
Whatever your center needs, there may be a Group Purchasing contract for it!
Everything from medical, dental and office supplies, practice software, office design, interpreting services, recruiting, and more. Visit their webpage for the latest newsletters and webinars, vendor info and more.

Where Innovation Sprouts: OPCA Peer Groups
OPCA recognizes that CHC staff members are the experts in their chosen fields. Our 12 peer groups are collaborative networks or forums where employees at our member organizations can speak others who hold similar roles or responsibilities to share knowledge, best practices, and tools.
One of the main goals of these peer groups is to provide a forum for knowledge sharing from clinical, administrative, and quality improvement teams from across the state’s 268 sites. Oregon’s CHCs all work toward the goal of health equity in their communities. For all of us to succeed, it’s imperative we have opportunities to connect, find support, and foster individuals’ professional development.
The majority of peer groups meet virtually on either a monthly, semi-monthly, or quarterly basis. Once a year, OPCA hosts the in-person All Peer Group Gathering, which rotates locations throughout the state. Groups with overlapping responsibilities, such as Communications Peers and HR Leaders, also have a chance to come together, collaborate and support one another.
Staff at OPCA’s member clinics may join relevant peer groups. Please contact us to join!






Behavioral Health Leaders
Clinician Leaders
Dental Leaders
Executive Leaders
Fiscal Leaders
HR Leaders






Medical Leaders
Nursing Leaders
Operations Leaders
Pharmacy Leaders
Communications Peers
HR Leaders
Inspired by Peer Group, OPCA Authors SB 608
In the 2023 regular session of the Oregon Legislature, OPCA introduced a bill to regulate pharmacy dispensing fees in fee-for-service Medicaid. OPCA became aware of the issue through knowledge sharing in our Pharmacy Peer Group. With input from FQHC pharmacists around the state of Oregon, OPCA drafted the bill to regulate the frequency and method by which pharmacist Professional Dispensing Fees (PDF) are adjusted.
The bill is brief, around 200 words, because that’s all we needed to fix a regulatory gap that caused significant issues for our members. Essentially, Centers for Medicare & Medicaid Services (CMS) doesn’t specify how frequently states should assess Professional Dispensing Fees (PDFs), and Oregon had not yet established a survey interval.
This lack of predictability raised challenges for pharmacies, especially those in rural areas struggling with revenue challenges. Without a set timeline, PDFs hadn’t changed in Oregon since 2018. With rising inflation and operating costs but no increase in the set fees for pharmacists’ services, the unadjusted payments didn’t reflect the time, material, and overhead costs of meeting the needs of patients.
“Access to pharmacy services is a critical component of closing the health equity gap. If we want pharmacies located in communities where people work and live and a pharmacy staff that reflects the community, we must adequately pay for those services,” said OPCA Policy and Government Affairs Director Marty Carty.
Senator Wlnsvey Campos (Democrat – District 18 – Aloha) sponsored the bill and introduced it on January 9, 2023. After six months of navigating the legislative process, the bill passed, and Governor Kotek signed it into law on June 7, 2023.
The bill is an example of how OPCA is uniquely poised to deliver impactful, precise, community-driven improvements to Oregon’s health care safety net.
AETC & OPCA Cross-Pollinate
In a November 2023 episode of the HIV Care Conversations Podcast, Dayna Kirk Morrison, Sr. Director of the Oregon AIDS Education & Training Center (AETC) Programs at OPCA, and Jill Coleman, Program Manager of the South Central AETC’s Oklahoma regional partner, shed light on the transformative impact of partnering with Primary Care Associations (PCAs). The discussion centers around the implementation of sustainable models of care for individuals with HIV, particularly addressing the challenges faced by clinics in remote regions.
 Understanding the Landscape in Oregon
Understanding the Landscape in Oregon
In Oregon, a state with 34 Community Health Centers, 5 centers, including Winding Waters, Mosaic Community Health, Neighborhood Health Center, and the HIV Health Services Center at Multnomah County, offer crucial HIV care services. Morrison notes a significant increase in new diagnoses, particularly in frontier areas, with trends among age groups 25-44 and rising rates within Indigenous, Black, Latine, and Pacific-Islander populations.
The conversation emphasizes the role of stigma, discrimination, and racism in these trends, prompting a shift from focusing solely on HIV and risk behaviors to considering broader factors such as social determinants of health and sexual and social networks.
 The Role of HIV Care Conversations
The Role of HIV Care Conversations
HIV Care Conversations is a podcast for healthcare providers treating and managing care for people with HIV in the United States. Through short conversations and interviews with field experts, this initiative aims to provide information, solutions, and resources to address existing and emerging issues in HIV care and prevention delivery to improve the health outcomes of those impacted by HIV.
 Partnerships for Community Impact
Partnerships for Community Impact
Morrison emphasized the pivotal role of CHCs and PCAs in increasing access to preventive services for smaller, rural populations. Integrating with OPCA not only provides an administrative link but also fosters a collective voice for transformation efforts in the healthcare system.
This collaborative approach extends beyond Patient-Centered Medical Home (PCMH) efforts to include Value-Based Payment (VBP) and other sustainable healthcare models. Advocacy for legislation supporting access to care and ensuring leadership alignment with workforce development is also highlighted.
“It is our job as a healthcare and public health workforce to make sure there are more tools and resources available to communities. This is where FQHC’s (CHCs) and Primary Care Associations can really play a big role in increasing access to preventative services for these smaller, more rural populations.”
-Dayna Kirk Morrison, Sr. Director of Oregon AETC Programs
APCM and Oregon’s CHCs: A 10+ year retrospective

OPCA’s Flagship Program
Conceptualized in 2011 and borne out of our health centers’ experience implementing a robust Patient Centered Primary Care Home model – which was extremely challenging under traditional fee for service payment – several health centers involved in the Safety Net Medical Home Initiative, and OPCA approached the Oregon Health Authority about modifying health center payment under the Prospective Payment System (PPS)— requesting more flexibility in payment to allow health centers to provide higher value care, rather than only churning out a high volume of visits.
Today, 20 of Oregon’s 34 CHCs, and 2 Rural Health Centers (RHCs) participate in this efficient and effective model of care, one of the first in the nation, optimizing health through services that engage patients.
Oregon’s APCM program was founded on the following principles:
- Accountability for outcomes (Triple/Quadruple Aim)
- Budget neutral
- Maintain patient access to care
- Patient-centered care (not tied only to face-to-face visit)
- Formal APM methodology
- Bridge to Value-Based Pay via social risk adjustment
Tracking Our Successes
Within the first 5 year of the program, APCM CHCs were meeting or exceeding CCO metrics (outcomes):
- Colorectal cancer screening rates increased from 50% to 55%
- Depression screening and follow-up rates from 57% to 74%
- Weight assessment and counseling for children and adolescents from 59% to 73%
By 2017, reliance on the traditional office visit was down and new care models implemented to meet patient need.
- DECREASED traditional office visits from 78 visits per 100 patients to 64 visits
- INCREASED number of reported Care STEPS from 5,605 to 99,344 (today, that number is over 1M)
Surviving Covid-19
 Under APCM, clinics are incentivized to provide high quality care but don’t have to rely on traditional in-office visits for funding. As a result, APCM clinics during the COVID-19 pandemic were able to provide the care their patients needed without a loss of operating funds. In fact, depression screening and follow-up during the first year of COVID-19 exceeded the baseline year, at 60% compared to 57% (baseline). APCM clinics also adopted during COVID-19 by adding COVID-19 vaccine administration as a meaningful engagement; carved out vaccine reimbursement from APCM; moved metrics to report-only status from 2021-2024; and enabled audio-only establishing visit for duration of the Public Health Emergency.
Under APCM, clinics are incentivized to provide high quality care but don’t have to rely on traditional in-office visits for funding. As a result, APCM clinics during the COVID-19 pandemic were able to provide the care their patients needed without a loss of operating funds. In fact, depression screening and follow-up during the first year of COVID-19 exceeded the baseline year, at 60% compared to 57% (baseline). APCM clinics also adopted during COVID-19 by adding COVID-19 vaccine administration as a meaningful engagement; carved out vaccine reimbursement from APCM; moved metrics to report-only status from 2021-2024; and enabled audio-only establishing visit for duration of the Public Health Emergency.
APCM Future Innovation Plans
 1: Onboard additional FQHCs and RHCs into APCM program and develop on-demand training for all participating CHCs.
1: Onboard additional FQHCs and RHCs into APCM program and develop on-demand training for all participating CHCs.
2: Streamline data and reporting. Although APCM is just one of our strategies for delivering high value care, our goal is for 100% of health centers to deliver high value care and to thrive in a value-based pay environment.
3: Advance towards VBC/VBP in tandem with state and the Network’s efforts.
4: Leverage success in SDoH (such as PREPARE/screening tools) to further state goal in equity and health related social needs (HRSN).
APCM Steering Committee Members

Matt Emery, Northwest Human Services
Blain West, Neighborhood Health Center
Gil Muñoz, Virginia Garcia Memorial Health Center
Sara Jade Webb, Wallace
Gail Nelson, Nehalem Bay Health Center
Mahea Kaeo-Wailehua, La Clinica
Marshall Greene, Mosaic Community Health
Chris Campell, Chair, Benton County Health Services
The Oregon Network For Community Health Centers Earns Approval for MSSP
 The Oregon Network of Community Health Centers (the Network) partnered with 15 federally qualified health centers to provide coordinated care for Medicare patients by establishing an Accountable Care Organization. This month, the ACO received federal approval to participate in a Medicare Shared Savings Program, which incentivizes providers to focus on patients’ health outcomes and cost reductions. This approach ultimately results in better health outcomes delivered at lower costs by prioritizing disease prevention and effective health screenings.
The Oregon Network of Community Health Centers (the Network) partnered with 15 federally qualified health centers to provide coordinated care for Medicare patients by establishing an Accountable Care Organization. This month, the ACO received federal approval to participate in a Medicare Shared Savings Program, which incentivizes providers to focus on patients’ health outcomes and cost reductions. This approach ultimately results in better health outcomes delivered at lower costs by prioritizing disease prevention and effective health screenings.
February 2024, the Oregon Network of Community Health Centers (the Network) earned federal approval for the organization’s Accountable Care Organization (ACO) to participate in a Medicare Shared Savings Program (MSSP).
The Network and its ACO affiliates serve just under 9,000 Medicare patients with essential primary, dental, and behavioral health care. The Network’s ACO members are Federally Qualified Health Centers (FQHCs) who face a multitude of challenges in balancing their operating budgets as they provide care to any patient, regardless of a person’s ability to pay or their insurance type. These constraints often inspire FQHCs to innovate new practices that make the delivery of health services more effective and more efficient.
The Network ACO’s federal approval for the MSSP is part of the organization’s larger plan to advance health equity for patients in Oregon. First, the Network purchased a license for the Arcadia data platform through funds received via a grant from CareOregon. The platform facilitates the aggregation of patient information to ultimately provide health centers with analytics to guide their clinical quality improvement efforts.
Next, the Network formed the ACO with participating FQHCs. “The formation of the Network ACO ensures that we can provide patients with the right care, at the right time for improved outcomes and interactions with healthcare,” said Network Director Carla Jones. “This is possible through case management, an emphasis on data performance, a strong focus on prevention, and through sharing best practices with each other. Additionally, an ACO avoids unnecessary duplication of services and prevents medical errors.”
The MSSP is another big step towards substantial cost savings, leading to upside earnings in the shared risk agreement with Medicare. “These savings allow clinics to provide patients with the best care possible,” said Jones.
The Centers for Medicare and Medicare Services (CMS) website explains, “When an ACO succeeds both in delivering high-quality care and spending health care dollars more wisely, the ACO will share in the savings it achieves for the MSSP. ACO formation also creates additional earning opportunities within the Medicare Fee for Service populations.
This project is emblematic of the Network’s core mission to bring together the experience and expertise of many health centers, thereby expanding collective power and increasing operational efficiency while also improving the quality of care for patients.
“We are thrilled to be a member of the first-ever Oregon Community Health Center Medicare Shared Savings Program ACO. This program will empower our team to provide more accessible, higher-quality primary and preventive care to Medicare beneficiaries throughout Northeast Oregon. Together, we’re improving the health of our communities.”
– Nicolas Powers, Winding Waters Clinic CEO
For more information about the ACO project, please contact Network Director Carla Jones, cjones@orpca.org.
 Promote the value of CHCs through branding and shared
Promote the value of CHCs through branding and shared  Advance APCM and VBP’s to
Advance APCM and VBP’s to  D
D
 Cultivate effective decision
Cultivate effective decision