According to the Oregon Center for Health Statistics, there are about 40,000 births annually. The journey into parenthood is one of life’s most transformative experiences, and it begins well before delivery day. Perinatal health services cover the critical period before, during, and after birth. From prenatal care and education to postpartum support, Oregon’s Community Health Centers provide perinatal services to ensure families have access to compassionate, comprehensive care at every step of the journey, and for the rest of their lives.
Today, OPCA is illustrating Oregon health centers’ role in supporting maternal and infant health, and how our team is partnering with the Oregon Perinatal Collaborative to support FQHCs delivering care to this population.
Resources, tools, and upcoming learning opportunities mentioned in this blog are available in the CHC Toolbox section.
Conversation about Perinatal Services
To understand the importance of perinatal health, Silke Akerson, Executive Director of the Oregon Perinatal Collaborative, shared:
“[T]he reason that maternal and infant health are so important in primary care is that maternal and infant health are the center and the foundation of community health overall. When people receive the care that they need during pregnancy, birth and postpartum, and when infants receive the care and support that they need, that sets people and the community up for lifelong health. And when people don’t receive the care that they need in pregnancy, birth, and postpartum, that can set up problems intergenerationally for the whole life cycle.”
Silke Akerson, MPH, CPM, LDM, Executive Director, Oregon Perinatal Collaborative
About 13 Oregon FQHCs offer direct perinatal care through their providers, and 85% of these health centers deliver care throughout the full pregnancy. For a fuller picture of how Oregon FQHCs support expectant parents, I sat down with care teams from Multnomah County Community Health Centers and One Community Health.

Connie Serra, MD
Medical Director
Esther Mondragon, RN
Perinatal Manager

Charlene Maxwell, FNP DNP
Dep. Medical Director
Toni Kempner, BSN, MSN, RN, ACRN
Director of Nursing
There is a common thread through all my conversations with One Community Health, Multnomah County Community Health Centers, and the Oregon Perinatal Collaborative: At the heart of perinatal care is trust.
For expectant parents and their families, finding a place to receive care is a deeply personal decision. Cultural values and lived experiences shape their decision, as well as whether they are confident that the health care provider will listen to their concerns. Federally Qualified Health Centers are well-positioned to deliver care to families because they reside in the communities they serve. Through compassionate, team-based care that honors the whole person, health centers build and cultivate trust.
Both One Community Health and Multnomah County Community Health Centers shared stories that reflect an eye for quality improvement, ensuring their patients received the best possible care. Because of their dedication to quality of care, their patients return time and time again, along with their children and loved ones. In addition to improving health outcomes during pregnancy and postpartum, health centers strengthen lifelong connections with the communities they serve.
Before ending our conversation, Silke Akerson expressed her excitement about working together with OPCA and FQHCs:
“[T]he Oregon Perinatal Collaborative started in this hospital-based, hospital-centered work, and at the time that made sense as a starting point because the peak of the iceberg issues that we needed to work on were at the time of birth in the hospital. But as we learn more from the Maternal Mortality and Morbidity Review Committee, so much of the prevention that can happen really needs to happen during prenatal care. And that’s with primary care providers, and that’s with Federally Qualified Health Centers. [Also] the majority of the maternal deaths that we have in Oregon and in the country happen in the postpartum period. And again, the people who are really touching on those lives in contact with those folks are primary care providers. “
Silke Akerson, MPH, CPM, LDM, Executive Director, Oregon Perinatal Collaborative
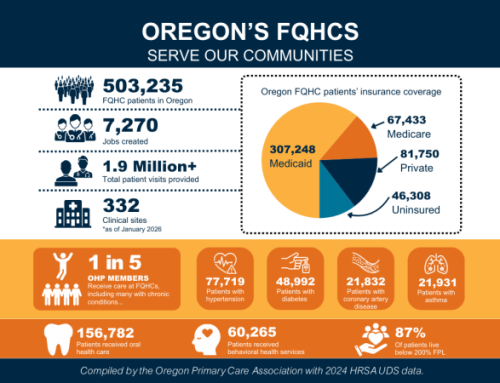
Federally Qualified Health Centers (FQHCs) are highly respected primary care providers. In addition to providing perinatal services, health centers enhance access to whole-person care. This access, in turn, promotes better health outcomes, which impact numerous aspects of the patient’s life. By establishing connections with individuals, their families, and the broader community, health centers deliver care to Oregonians throughout their lives.
Attend the Perinatal Health Summit

Whether your health center provides comprehensive prenatal care, primarily supports people during the postpartum period, or falls somewhere in between, this event is designed for you!
The Summit will explore Oregon’s maternal health landscape and offer practical, actionable strategies for improving outcomes across the perinatal continuum.
If your clinic serves people of reproductive age in any capacity, this Summit will offer tools, partners, and ideas to strengthen care and improve maternal health outcomes.
Questions? Contact Joanna Peterson at jpeterson@orpca.org.
CHC Toolbox
Related Resources