The Oregon Primary Care Association (OPCA) is a non-profit membership association for the state’s federally qualified health centers (FQHCs) and look-alikes. We generate data-driven insights into operational challenges, shape evolving health policy, and provide technical assistance to FQHCs and look-alikes in Oregon.
Our members deliver integrated primary, dental, and behavioral health services to more than 470,000 Oregonians. In addition community health centers work to help patients improve the circumstances of their lives and develop healthy behaviors through services like job training, literacy education, and connection to resources for affordable housing and healthy food.
OPCA’s Six Strategic Domains
2024 – 2026

1. Drive population health and CHC value through partnerships, policy, public affairs, and data.

2. Advance Care and Payment Models that support the evolving needs of Oregon’s CHCs.

3. Build CHC capacity for effective population health through increased engagement, quality improvement, data & analytics, and shared programming.

4. Develop and support an engaged workforce to meet current and emerging needs, reflecting communities we serve.
5. Bolster and reinforce governance (OPCA Board) development ensuring OPCA is centered in its mission, vision, and values.

6. Build robust operational and financial organizational infrastructure
A Year of Momentum
Welcome to OPCA’s 2024-2025 Annual Report
Dear Friends, Members, and Partners,
OPCA is now halfway through our three year strategic plan. While the path forward has been filled with surprises, our team has made steady progress that’s quickly turning into momentum that will sustain our next phase of work.
As you’ll see in the following pages of this report, each department at OPCA has accomplished somethin extraordinary over the past fiscal year.
First, our Alternative Payment and Advanced Care Model (APCM) has always been about measuring what matters. In 2025, we took more than a decade of data-driven insights and our value-based pay philosophy into a new format for use beyond our clinics. Our Care STEPs model is now in use by CareOregon. It’s a breakthrough not only in care delivery, but in how we recognize, reward, and replicate what community health centers do best. Our Policy team has been busy shaping state and federal law. In just two years, we’ve grown from co-authoring our first bill to advancing three and passing two this session. Right before the 2025 legislative session ended, OPCA’s bills, HB 2385 and HB 3409 became law and further protect CHCs’ 340B benefits. Beyond Oregon, our member CHCs showed up in force at Washington DC this year for PNI, where CHC leaders came to speak with national leaders about the importance of supporting community-based health.
Our Programs team also brought unprecedented energy to member engagement this year. We held our second annual conference bringing together our members and partners from across the state and nation for innovative learning and conversation. We also continued offering training and technical assistance to support health centers in a wide range of areas including, but not limited to, value-based care, operations, compliance, workforce, and clinical skills, including HIV/STI treatment and prevention. We also convene leadership and affinity groups for our members to build meaningful collaborations that drive quality improvement and statewide innovation.
Our subsidiary, the Oregon Network of Community Health Centers began in 2020 and is now a full-fledged health data ecosystem. With all 15 participating health centers fully onboarded and a federally approved ACO, Oregon’s CHCs finally hold the keys to their own data and their own future.
Internally, our HR department has demonstrated that retention begins at the interview table. And our Finance team ensured we grew not just in size, but in
sustainability, with more diversified funding and smarter operations to match our ambitions.
At OPCA, we’re not waiting to be invited to the table — we’re setting it. And we’re making sure Oregon’s community health centers have a seat, a voice, and the data to lead the conversations.
Thank you for walking this path with us. The road to a healthy Oregon is long, but we are making significant progress together.
Yours in solidarity,
Joan Watson-Patko

Table of Contents
- 2024-2025 Annual Report
- OPCA’s Six Strategic Domains
- A Year of Momentum
- From the Clinic to the Capitol
- Legislative Session Stats
- Million+ Steps Toward Better Care
- 2024 Events and trainings at a Glance
- EXPLORE OPCA TRAINING & TA RESOURCES
- Thank You to Our Generous Sponsors!
- Keeping Humans Central in HR
- Building Financial Infrastructure
- The Network’s Data Platform For Health Centers, By Health Centers
- Congratulations to OPCA’s 2025 Annual Award Winners!
From the Clinic to the Capitol
Doubling our Legislative Impact Through New, Member-Led Committee
Policy momentum takes more than meetings. It takes trust, strategy, and a unified voice. In just two years, OPCA’s policy team has gone from supporting legislation to shaping it. This year, that momentum produced real protections for Oregon’s CHCs and the patients they serve.
In 2023, OPCA’s first-ever bill, SB 608, became law and resulted in pharmacy dispensing fees for FQHCs increasing from $14.30 to $20.86 in fee-for-service Medicaid prescriptions. This victory helped inspire our members to get more invested than ever in the legislative outcomes and processes.
In 2024, OPCA launched the Policy Development, Research, and Review Committee (PDRC) to quickly gather information and form consensus with member health centers about how to address emerging policy issues as a unified voice.


This new committee reviews, analyzes, and makes recommendations to the OPCA Board of Directors on legislative issues related to health care, public health, related social policies and regulatory changes and more. PDRC members also work collaboratively with OPCA’s professional groups and legislative liaisons to get a clear view of issues facing Oregon CHCs.
Photo: Representatives Bonamicci and Dexter on a visit to OutsideIn to better understand Oregon’s CHCs. This connection was one of many between legislators and Oregon CHCs this past year.
| BILLS OPCA SUPPORTED | Status |
|---|---|
|
Expand Investment in Healthcare Workforce SB 27 + SB 283 – Included a $9 million investment in workforce recruitment and retention efforts at FQHCs |
Failed |
|
Support for School-Based Mental Health Services HB 2729 – Directed OHA to establish a grant program expanding school-based mental health and substance use services; included a study on reimbursement models for mental health services delivered by school-based health centers. |
Failed |
|
Ensure Sustainable Funding for School Health Centers HB 3169 – Required annual grant funding for school-based health centers to be adjusted for inflation. |
Failed |
|
Restrict Flavored Tobacco Products SB 702 – Aimed to curb youth vaping by banning the sale and distribution of flavored tobacco and inhalant delivery products, with limited exceptions. |
Passed! |
| BILLS OPCA OPPOSED | Status |
|---|---|
|
Pilot Telehealth Programs in Schools HB 2577 – Proposed a pilot program to evaluate the impact of school-based telehealth on student access to care. However, it was written in a way that no Oregon SBHC would have qualified for funding. |
Failed |
|
Address Gaps in Dental Reimbursement HB 2597 – Sought to raise Medicaid dental capitation rates; however, FQHCs would not have benefitted due to the PPS structure. |
Failed |
Legislative Session Stats
3,385 BILLS INTRODUCED
669 PASSED
OPCA TRACKED
306 BILLS
OPCA WROTE 3 BILLS
2 PASSED
OPCA SUPPORTED 4 BILLS
1 PASSED
OPCA OPPOSED 2 BILLS
BOTH FAILED
Big Wins for Oregon CHCS
Two bills championed by OPCA and Oregon’s health centers, HB 2385 and HB 3049, passed. This marks a major step forward in protecting the integrity and financial viability of the 340B program.
 HB 2385 prohibits restrictions on the use of contract pharmacies in the 340B program.
HB 2385 prohibits restrictions on the use of contract pharmacies in the 340B program.
This bill enshrines into Oregon law critical protection for FQHCs, ensuring they can continue using contract pharmacy arrangements to serve their patients.
HB 3049 prevents PBMs and manufacturers from requiring FQHCs to use unique claims identifiers.
Claims identifiers are an administrative burden often used to deny 340B claims or redirect savings. This bill reinforces health centers’ ability to operate the 340B program effectively and without unnecessary barriers.
These bills represented more than policy victories: they were an opportunity to amplify our voices, teach lawmakers about our mission, and highlight the unique challenges FQHCs face within the broader healthcare system. Our success underscores the strength of coordinated ongoing advocacy.
Million+ Steps Toward Better Care
Learn How Our APCM Program is Leveling Up
OPCA’s Alternative Payments and Advanced Care Model (APCM) has served patients and providers at CHCs for more than a decade. Now, at the request of Coordinated Care Organization (CCO) CareOregon, OPCA is building the lessons of APCM’s Care STEPs into a new product for non-members. OPCA’s latest venture in payment innovation enables CareOregon to adopt APCM’s strategies across Oregon’s health landscape. In the future, OPCA plans to bring Care STEPs to more CCOs for an even greater impact.

WHERE WE STARTED: Alternative Payment and Advanced Care Methods Bring Better Health at Lower Costs

In 2013, OPCA, the Oregon Health Authority (OHA), and Oregon’s Federally Qualified Health Centers (FQHCs) built a bold new approach to healthcare delivery: the Alternative Payment and Advanced Care Model (APCM). Designed to align payment with the actual value of care delivered, APCM shifts the focus of health care billing from the volume of patients’ visits to the quality of care delivered. This approach empowers health centers to meet patients’ needs through team-based, innovative, and often non-traditional services.
APCM incentivizes health centers to focus on helping people stay healthy, not just treating people when they’re sick. Services like personal and group wellness education, dental and behavioral health referrals, and screenings for chronic health conditions all help patients build a foundation for long-lasting health.
The quest for the perfect balance between health outcomes with service costs continued as OPCA and participating health clinics worked together to aggregate data and share best practices which consistently led to better health outcomes for patients.
WHAT WE LEARNED: OPCA and Participating CHCs Identified 18 Provider Actions Which Consistently Created Better Outcomes for Patients
By 2017, OPCA’s APCM team formalized a new way to document and recognize the spectrum of services needed for population health: Care and Services That Engage Patients, aka Care STEPs. OPCA built the STEPs with OHA’s approval and with coordination from OCHIN.
A Care STEP is a direct interaction between a patient (or their family/representative) and a health center team member. Care STEPs can be grouped across four categories: new visit types; education and wellness; care coordination; and barrier reduction. The Care STEPs model ensures that prevention, outreach, and accessibility-focused work count just as much as clinical encounters.

WHERE WE’RE GOING NEXT: OPCA is Preparing to License Care STEPs to More Coordinated Care Organizations to Meet Statewide Financial and Population Health Goals.
In 2024, CareOregon piloted the use of Care STEPs as an incentive metric. CareOregon is working with select FQHCs to track patient engagement and access, as both are critical components of value-based care (VBP). This pilot aims to determine how Care STEPs can support statewide VBP policies.
OPCA created a special onboarding program for non-APCM teams in support of this effort. At the same time, OPCA’s Accountability Workgroup is continuing to strengthen the data infrastructure that underpins APCM and VBP efforts. This ensures that every Care STEP delivers a meaningful patient interaction and advances the larger, data-informed push toward better care and smarter spending.
With Care STEPs on the verge of becoming a license-ready product, OPCA plans to bring this innovation to new partners and payers as a scalable solution.
More than one million steps later, the path ahead is clear: supporting and documenting meaningful interactions between providers and patients improves overall population health while also decreasing costs through a focus on prevention.
Interested in joining APCM and/or utilizing Care STEPs?
Email Danielle Sobel (Dsobel@orpca.org) for more information!
2024 Events and trainings at a Glance
OPCA offers a comprehensive suite of programs that support Oregon’s community health centers in delivering high-quality, whole person care. Our work aligns with federal HRSA expectations while remaining responsive to the changing needs of our members, bolstered by grant funding and strong cross-sector partnerships.
We focus on core areas such as behavioral health integration, workforce development, value-based care, and system transformation. Through targeted training and technical assistance, we create opportunities for shared learning and practical solutions. Our statewide programs are designed to foster innovation, strengthen collaboration, and advance the collective capacity of Oregon’s FQHCs.





Behavioral Health Leaders

CHW Supervisors

Comms Leaders

Dental Leaders
Executive Leaders

Fiscal Leaders

HR Leaders

Medical Leaders

Nursing Leaders

Operations Leaders

Pharmacy Leaders

Quality Improvement Collective
Interested in joining a peer group? Fill out this form!
EXPLORE OPCA TRAINING & TA RESOURCES
Leadership Groups
OPCA convenes 12 groups throughout the year that meet for learning and discussion around shared topics of interest. These groups include a Quality Improvement Collective and Population Health Workgroup that focuses on metric management and best practices sharing using health center data and case studies.
Value Based Care Collective
OPCA offers a suite of value-based pay (VBP) training and resources, including a newly launched resource repository. This year, in addition to our APCM Forum, which was for APCM member clinics only, we held 3 additional VBP trainings that were open to all OPCA members. These trainings focused on population health management and care team integration.
Health Center Operations
Workforce Program
- Leadership Trainings
- Staff Safety Trainings
- Health Professions Education & Training Pilots
- Career Pipelines Convenings
Health Center Compliance
- Emergency Preparedness Annual Convenings
- Support for expanding sites and/or services
- Group Purchasing
Clinical Improvement Community
- HIV/ STI Program
- Annual Cancer Screening Training
- Quality Improvement Collective
- Annual Provider Communications Trainings – Certificate Training to meet PCPCH Requirement 6.E.0
- Polysubstance Use Disorders Workgroup for FQHCs
- Annual Intimate Partner Violence Screenings
- Maternal Health Strategy Sessions
- Diabetes & Oral Health Screening & Metrics
AVAILABLE NOW: Leadership Resources Repositories
OPCA has launched four new resource repositories on our Member Portal. CHC employees can login to OPCA’s member portal at orpca.org to access the following repositories:
- Leadership Resources
- Emergency Preparedness Resources
- Board of Directors Resources
- Value Based Pay Resources
(Please note: you must be logged into our Member Portal to view these resources)
Thank You to Our Generous Sponsors!
In 2024, OPCA Doubled Annual Conference Sponsorships to Reduce Costs for Members
OPCA’s 2025 Annual Conference theme, Mobilizing Health Care Transformation, focused on actionable initiatives to improve health outcomes and transform healthcare systems for all Oregonians. Attendees included key decision-makers and partners from local and national health centers, with sessions featuring OPCA-led training and advocacy opportunities. This year was our biggest conference yet, with four days of programming for attendees!
Conference guests were encouraged to follow one of three focus tracks for breakout sessions: Clinical Innovations, Operations and Leadership, and System Transformation.
Keynote and Plenary Speaker Spotlight

Dr. Erin Taylor
PacificSource CCO

Dr. Bruce Goldberg
OHSU

Dr. Emma Sandoe
OHSU

Colleen Meiman
National Health Policy Advisor

Laurel Durham
Oregon Perinatal Collaborative
20 Sessions
28 Speakers
199 Guests
9 Sponsors
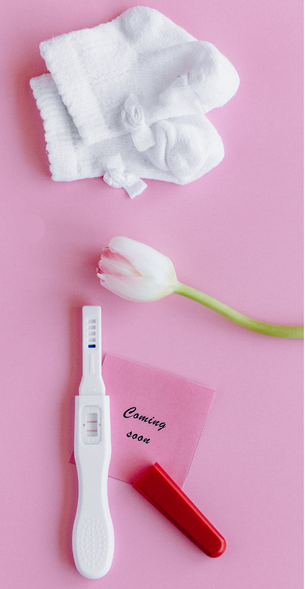
Advancing Maternal Health Through a New, National Initiative
In January of this year, HRSA announced a “Landmark Year of Enhancing Maternal Health,” and allocated $19 million nationally to health providers and partners to study and identify key drivers of maternal mortality.
At the Annual Conference, OPCA launched the new Oregon Maternal Health Collaborative. The kickoff session brought together CHC health providers to gain a shared understanding of the issues and begin envisioning best practices that can be implemented statewide. The Oregon Perinatal Collaborative kicked off the day with a keynote presentation. Notably, a sampling of Oregon’s 2018-2021 maternal deaths revealed that of 32 pregnancy-related cases, 72% of those deaths were potentially preventable (compared to 80% nationally).
The kickoff meeting included feedback from four CHCs, OHA, the Oregon Perinatal Collaborative, Willamette Health Council, and Comagine Health. OPCA is now working on an environmental scan to build the full picture of maternal health at Oregon FQHCs. The results of this scan will inform content for an upcoming maternal health symposium in 2026.
Keeping Humans Central in HR
The OPCA Human Resources’ Unique Approach to Hiring Brings in and Retains High-Quality Staff
People power momentum. That’s why OPCA has made empathy-centered hiring and long-term staff support a cornerstone of our organizational strategy. We know that the best way to serve our members is by first building a thriving internal team.
As an organization that celebrates people, centers accessibility, and seeks new paths forward on our journey towards health for all, OPCA’s makes space for candidates of all backgrounds in our hiring practices.
For each interview, we:
- Provide candidates with a copy of the interview questions the night before, a guide on how to best share their experiences, and OPCA’s values;
- On the day of the interview, provide the candidate with a hard copy of the questions to help keep them grounded;
- Assign a notetaker to jot down responses so that the hiring team and candidates can focus on the conversation;
- Share an overview of the position & organization to give candidates context;
- Ask questions both related to the job and the candidates’ values (i.e. what brings them joy);
- Allot time for candidates to ask the team questions;
- Walk candidates around the office to showcase our environment (like our light-filled space and thriving plants)
70% of OPCA’s staff have been with the organization for 3 years or more.
Building Financial Infrastructure
Every leap we made this year was made possible through a solid financial foundation. OPCA’s finance team ensured that our growth was supported through increasingly diversified revenue sources, improved operational efficiency, and new strategic partnerships.
OPCA’s Revenue Sources
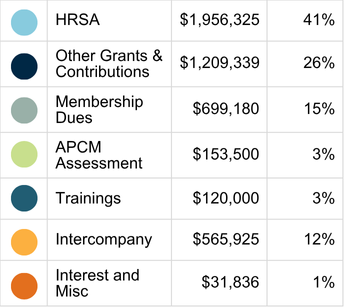

Grant Highlights

$807,433 for the HIV/STI Program

$177,083 for HRSA Grant for Maternal Health

$74,967 OHA grant for data collection project
The Network’s Data Platform For Health Centers, By Health Centers
OPCA and the Network are building digital infrastructure for Oregon’s CHCs to have the insights they need to deliver optimal care at low costs.
“Accountants and policy leaders need data to understand the value of what we do. However, Oregon’s health centers didn’t have the infrastructure to collect, analyze, and use that information themselves to improve patients’ health outcomes. Now, we do.”
– OPCA Data Director Simon Parker-Shames
For several years, the Oregon Network of Community Health Centers has been building the foundation for a missing piece in the CHC landscape: a data platform owned and governed by the health centers themselves.
“In so many statewide initiatives around the nation, we saw data systems built around the needs of insurers or external administrators,” said Network Director Carla Jones. “This time, we said: what if the health centers got to decide what mattered?”
In 2023, the Network began building a platform specifically designed to empower CHCs to succeed in a value-based care environment. Now, every single one of the 15 health centers that signed up for the platform has successfully onboarded their staff members into the new system. Onboarded staff members underwent extensive trainings to understand how to properly upload, access, interpret, and protect patient data.
Participating clinics now have access to a growing trove of insights. The platform stores multiple types of patient information, i.e. Medicare status, emergency department usage, and electronic health record (EHR) data. By storing multiple record types into a single, high-end software, community health centers can get a much clearer sense of their patients’ and their communities’ needs.
The data platform also hosts critical information for the Network’s Accountable Care Organization (ACO), which received federal approval in early 2024. With five years of Medicare data covering more than 10,000 patients and comprehensive EHR data from 12 Network member clinics, the ACO is also on strong footing to better understand their patients and deliver optimal care.
Next, the Network plans to expand partnerships with payors like OCHIN and bring in data from the Alternative Payment and Advanced Care Model (APCM) program to further strengthen population insights and performance evaluation.
By the end of the CareOregon contract period, the Network aims to have EHR data from every participating clinic housed within the platform. This next milestone will pave the way for smarter care delivery and more accurate payment models.
CareOregon’s Chief Medical Officer Dr. Amit Shah sees this project as essential. “A stronger Community Health Center Network means better health outcomes and improved health access across Oregon. That’s why CareOregon is proud to partner with the Network. As the Oregon Network grows, so will our collective impact.”
Already, the benefits are tangible. Onboarded health centers can use the platform to stratify the data they collect as part of their work with OPCA’s Quality Improvement Collective (QIC) to identify disparities and implement community-led interventions. Members of the QIC already reports above-average scores across nearly every major quality metric, including colorectal screening, urgent care access, and chronic condition management like diabetes and hypertension.
“It’s not just about metrics; it’s about impact,” said Jones. “Participating health centers report strong improvements in behavior change and confidence scores, underscoring the real-world value of having the right data, in the right hands, at the right time. As Oregon’s community health centers continue to move from volume to value, the Network’s new data platform is a major turning point.”
Congratulations to OPCA’s 2025 Annual Award Winners!
Since 1988, OPCA has recognized more than 200 Community Health Center innovators who went above and beyond to support their patients and colleagues. By highlighting the inspirational stories of excellence in Oregon’s Community Health Centers, OPCA celebrates the values which guide community and state transformation of primary, dental, and behavioral health care. When we learn how somebody made a difference in their community, we also learn important practices for replicating their results.
Click on the winners’ photos below to see our blog posts about their exceptional work in their respective fields!
Annual Awards’ Honorable Mentions
Jonathan Lewis
La Clinica
Nan Zunkel
Multnomah County
Health Department
Shawnacy Herron &
Echo Wooten
La Pine
Nara Northwest
Dental Team
Chris Campbell
Benton Linn
La Clinica Community Builders
Multnomah County HIV Health Services Center
Kristen Weidner, Alynn Vienot Hayes, Carolyn Tziu
Neighborhood Health Center
Stephanie Silleck, Ari Rapikin, Bethany Stairs
Wallace
Dr Jay Richards
Aviva Health
Katie Whipple
Clackamas Health Centers
Kendra Newbold
Coast Community Health
Kellee Borsberry, Justin Davis, Kevin Holloway, Layni Kaplan, and Peter Buekea
Northwest Human Services