One in three adults are living with prediabetes and may not know. This is often the case as the onset of diabetes or prediabetes may present as A1c levels that aren’t high enough to be diagnosed as diabetes. To prevent the progression of diabetes, the National Diabetes Prevention Program (DPP) incentivizes the enrollment of at-risk populations, equipping patients with health and hygiene practices to manage their condition. Management of diabetes isn’t just about counting carbs or checking blood sugar; it’s about having the right support system. For many Oregonians, that support starts at their local community health center, where care teams help patients navigate the challenges of diabetes with compassion and teamwork.
The question for today is, what does the Diabetes Prevention Program look like in the Oregon Health Safety Net? In this post, OPCA is focusing on the delivery of the National DPP in Oregon, challenges health centers encounter, and an inside peek at DPP implementation at Adapt Integrated Health.
Resources, tools, and upcoming learning opportunities mentioned in this blog are available in the CHC Toolbox section.
Conversation about Diabetes Prevention
In our state, the Oregon Health Authority, Comagine Health, Oregon Health & Science University, Oregon Medical Association, Oregon Wellness Network, and OPCA have formed a Diabetes Prevention Alignment Workgroup. With an overall mission to leverage, align, and coordinate strategies and resources to increase engagement in the National DPP, the workgroup hopes to see a lower prevalence and burden of Type 2 diabetes in Oregon. This vision especially applies to adult patient populations who are disproportionately impacted. Lavinia Goto, with the Oregon Wellness Network, is participating in the workgroup and shared:
“ [It’s] very unique. I tout it every time I go to a national conference because it is so unusual, and it’s been extremely helpful in getting the program to where it is now. [Our workgroup] has helped provide the infrastructure and address some of the policy issues surrounding the introduction of a program like DPP in the state. Another advantage is that while we focus on [National] DPP, it could really be applied to any prevention program.”
To understand the delivery of the National DPP services in Oregon better, Lavinia shared insight into her experience assisting primary care providers, especially Federally Qualified Health Centers.
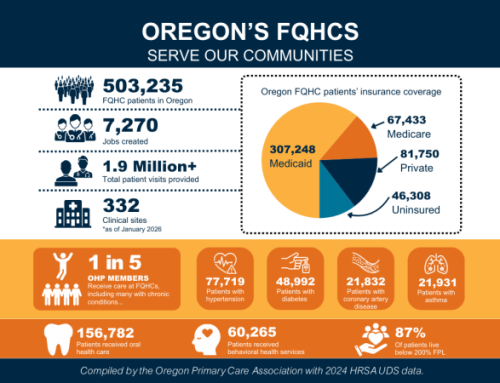
At OPCA’s Quality Improvement Collective, the group examines quality measures set at the state and federal levels, and highlights the top-performing health centers. In 2025, Valley Family, Winding Waters, and Mosaic Community Health lead the pack in diabetes and hypertension control. On a national level, four health centers were recognized by HRSA’s Health Center Program and received National Quality Leader Badges in Diabetes Health: Lincoln County Community Health Centers, Northwest Human Services, Rogue Community Health, and Adapt Integrated Health Care.
To understand the National DPP delivery at a health center, I spoke with care team members and staff at Adapt Integrated Health Care.
Implement the National Diabetes Prevention Program at your Health Center
Chronic disease prevention is at the core of community care. Community Health Centers understand their communities, their patients, and the most effective ways to engage both in managing their health. By adopting strategies like the National Diabetes Prevention Program, health centers can lower the prevalence and burden of Type 2 diabetes among adults in Oregon.
Expanding National DPP access is a chance to equip patients with healthy lifestyle practices, while strengthening the long-term health and wellness of the communities we serve. To help primary care providers with data collection and reporting for National DPP, the Oregon Wellness Network can assist in the following way:
For Community Health Centers eager to participate in National DPP, please get in touch with Lavinia Goto at the Oregon Wellness Network. You can contact her directly at lavinia.goto@nwscs.org or call 1-833-ORE-WELL (833-673-9355). Both DPP participants and FQHCs can use the help line if they have any questions about program delivery assistance or where to find the nearest class.
CHC Toolbox
Related Resources