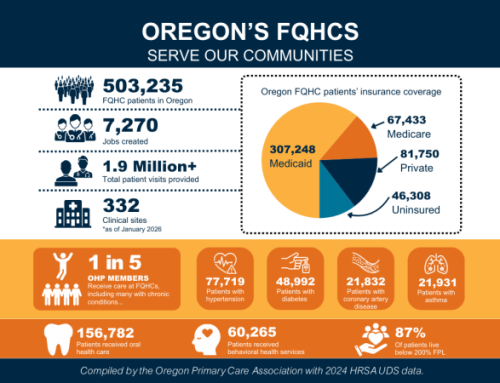
Community Health Centers (CHCs) are trusted primary care providers in Oregon’s health safety net. As a result, many health care entities and partners look to CHCs as trailblazers, innovators, and collaborators. At the same time, health centers are accountable to payors to reduce the total cost of care while spearheading efforts to strengthen population health. Meeting these expectations places an immense burden on community health centers.
IntegratOR (also known as the Oregon Network of Community Health Centers) collaborates with health centers to leverage their collective power. As one voice, members can negotiate better value-based care agreements by utilizing dependable data systems and quality improvement initiatives.
In this post, OPCA highlights IntegratOR’s partnership strategy to position its Accountable Care Organization and Data Platform as ideal tools in addressing anticipated changes in health policy. Resources, tools, and upcoming learning opportunities mentioned in this blog are available in the CHC Toolbox section.
Conversation about Partnerships
Community Health Centers deliver primary care to their communities regardless of an individual’s insurance status or ability to pay. This raises the question: How do health centers fund health services and programs? The sustainability of CHCs depends on financial arrangements with payors. Payors are entities that cover or reimburse the cost of health services provided by primary care settings. As a means to ensure quality and control, payors will:
For health centers, an Accountable Care Organization (ACO) is a valuable resource to assess the quality, cost, and overall care of defined patient populations. In early 2024, IntegratOR formed an ACO, named EnactOR. Upon its formation, EnactOR received approval from the Centers for Medicare and Medicaid Services (CMS) to participate in the Medicare Shared Savings Program (MSSP).
ACOs participating in the MSSP commit to managing both the quality and total cost of care for a specific group of Medicare beneficiaries. When they meet quality standards and keep costs below an established benchmark, ACOs earn a portion of the savings. EnactOR, with Medicare attribution and claims data representing around 8,000 patients, along with comprehensive EHR data from 12 member clinics, earned shared savings in its first year of performance in the MSSP.
To gain a deeper understanding of existing partnerships, I had the privilege of sitting down with Carla Jones, Network Director of IntegratOR.

Carla Jones, Network Director

IntegratOR is deeply committed to strengthening partnerships with providers to identify pain points and propose effective solutions. A complementary service to the ACO, EnactOR, is VisualizOR, which is a data platform built by and for Oregon’s community health centers. Read the post, From Insight to Impact: Strengthening Population Health, to learn how CHCs gain insight into the individual and collective performance of health centers.
Access Population Health Resources
Community Health Centers are a cornerstone of primary care in Oregon. For over 60 years, their reliability and dedication to delivering care to Oregonians in the most need have secured their position as respected primary care providers. However, the changing health policy landscape and the increasing challenges in health care delivery pose significant challenges.
Central to improving population health, IntegratOR offers a sustainable, long-term solution to enhance advanced access to care and support the financial and clinical success of CHCs. Through collective bargaining power, quality improvement initiatives, and centralized services, member clinics can navigate anticipated challenges and continue their mission of delivering care to those in need.
To be a part of this transformation and learn more about IntegratOR and its services, contact Carla Jones, Network Director, at cjones@orpca.org.
CHC Toolbox
Related Resources